By Tushad Driver | January 11, 2019
Original Article
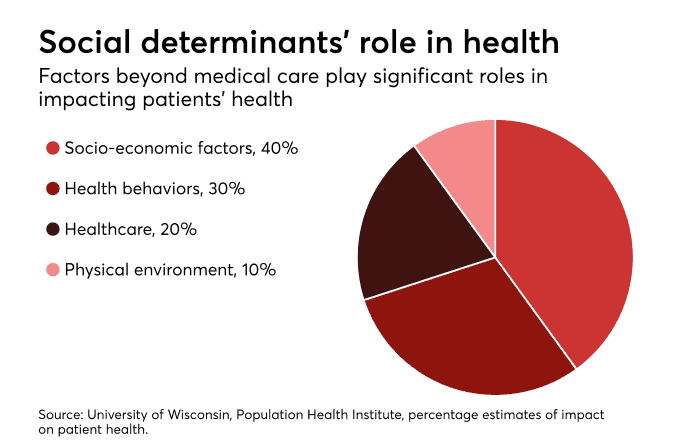
A large body of research now confirms what health practitioners have long known—social determinants like access to transportation and nutritious food—have a significant impact on patient outcomes.
A widely cited study by ICSI has estimated 80 percent of an individual’s health is influenced by social determinants. Consequently, a survey by Change Healthcare found that 80 percent of payers are investing in tools to address social determinants of health. Payers, hospitals and other healthcare organizations are eager to act on these recent findings and strategically invest in new social and community programs.
The Centers for Medicare and Medicaid Services (CMS) announced in May that Medicare Advantage plans could, in 2019, expand the health-related benefits they offer. If anything, Medicare Advantage would just be catching up to that reality.
However, increased innovation, investment and awareness alone won’t translate into meaningful cost reduction and improved patient outcomes, unless social determinant data collection and management are fully prioritized to get the insights needed.
For instance, who is best served by quick access to transport? Or to fresh, nutritious food? And how would that translate into downstream medical cost savings and improvements in health outcomes? It doesn’t matter what social determinants program you invest in, if you’re not equipped to get insights from that data, you almost might as well not do it.
The services provided under the banner of social determinants—community health visits, transportation services, fresh meal programs, gym membership and more—are also relatively less expensive, compared with the services of clinical practitioners. A gym instructor has a much lighter debt burden associated with their credentialing process than a physician coming out of medical school. But that doesn’t mean their social determinant benefits can be given out like candy or a novelty to dress up a health plan as hip and cool, with a dusting of quantitative evidence.
Even when analytics operations exist, most are tailored for reporting or retrospective analysis. That limits the insights into the value of social determinants and how you evolve them. Payers and providers are working on new multi-variant predictive and inferential ways of using data to diagnose, predict and prescribe, not just describe the past. Meaningful, actionable insight involves translating the “what happened” to “what will happen, and what do I do about it?”
This is the common tale across healthcare today—innovations are only as good as the data and your ability to get actionable insights from that data. As we move into 2019 what will be most interesting will not be what will constitute social determinants-related activity, nor how much is invested in them, but how payers in particular are measuring their effectiveness.
Part of this requires integration of payer and provider data with publicly available or syndicated social determinants data. Payers’ and providers’ own systems tend to be siloed.
Healthcare data sets are complex, fragmented and often, of poor quality and usability. The process of ingesting, loading, cleaning, transforming, linking and reporting itself continues to be overwhelming for resource-strapped teams. Let alone analyzing and generating insight to drive business operations; a proliferation of proprietary standards and tools also adds to the complexity.
An open-source cloud-based platform delivering “analytics as a service” can help mitigate much of the complexity and streamline the “data to insight” lifecycle. An “Analytics as a Service” platform can automate large parts of the ingestion and data quality process, provide easier sharing and collaboration, improved security, deeper analytical and data visualization capabilities, at significant scale.
A data and analytics strategy that can blend social determinants data at scale is critical to generating an analytics-ready data set that is primed for insight. Without this, social determinants will just be another item thrown into an ever-growing and unwieldy healthcare “big data” world, generating even more noise and less insight.
Tushad Driver is vice president of products at Gray Matter Analytics.