Achieve Optimal Outcomes and Cost Savings with Gray Matter Analytics Solutions
Improve care coordination
Ensure members receive coordinated and efficient care that leads to better health outcomes and reduced costs. With CoreTechs®, easily track and monitor member interactions with providers, identify gaps in care and highlight outreach opportunities by efficiently screening data. Suggest interventions based on measures’ eligibility and compliance, demographics and practice or provider information. Access quality and utilization measures reports, compare performance across practices and prioritize underperforming providers for targeted intervention.
Reduce avoidable spend
Reduce costs and maximize revenue potential while improving quality of care. Use the data-driven CoreTechs® solution to identify high-risk populations, track utilization patterns and manage costs by allocating resources to areas where they will have the greatest impact. Inform payment model creation and incentive development to enhance primary care services, prevention and disease management with minimal gaming. Even incremental gains can eliminate downstream effects on cost and broaden participation in value-based care.
Elevate quality of care
View performance against financial, utilization and quality measures across multiple contracts to engage providers, efficiently manage service to members and support delivery of the highest quality of care possible. Monitor and measure quality of care, assess program and intervention effectiveness, identify areas for improvement and ensure that care providers are meeting standards and promoting health equity and population health.
Promote better health outcomes
Use integrated claims, utilization and other data to understand provider progress against set goals and stay on track of HEDIS with CoreTechs®. Achieve better health outcomes for your members by intervening early. Our analytics help identify potential problems for members with rising risk before a critical event happens. Plus, access to meaningful clinical quality information enables identification and elimination of low-value services so services that have a greater impact on outcomes and patient goals of care may be emphasized.
Manage compliance with standards
Mitigate potential risks and stay compliant with regulations and reporting requirements, including Medicare Advantage and Medicaid cost measures. Gray Matter facilitates reporting and ensures that benefit providers are meeting all regulatory requirements so they can focus on improving care and outcomes for your members.
Maximize your revenue potential with contract-level insights – uncover hidden value, prioritize revenue-generating opportunities and mitigate potential risks.
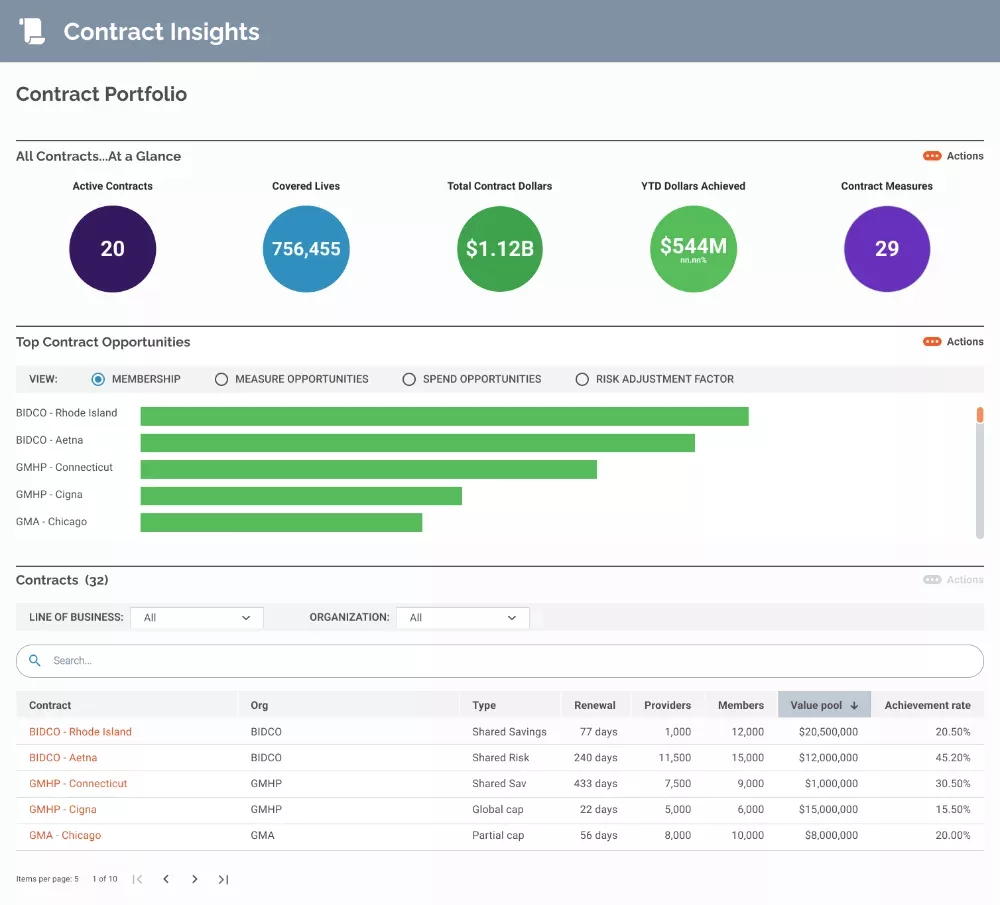
- Contract performance analytics: View performance against financial, utilization and quality measures across multiple contracts.
- Contract data integration: Use integrated claims, utilization and other data to understand holistic performance.
- Configurable analytic insights: Quickly and easily view contract performance and insights to trends and improvement opportunities through customizable dashboards.
Monitor provider progress against set goals, stay on track of HEDIS measures and drive improved patient outcomes.
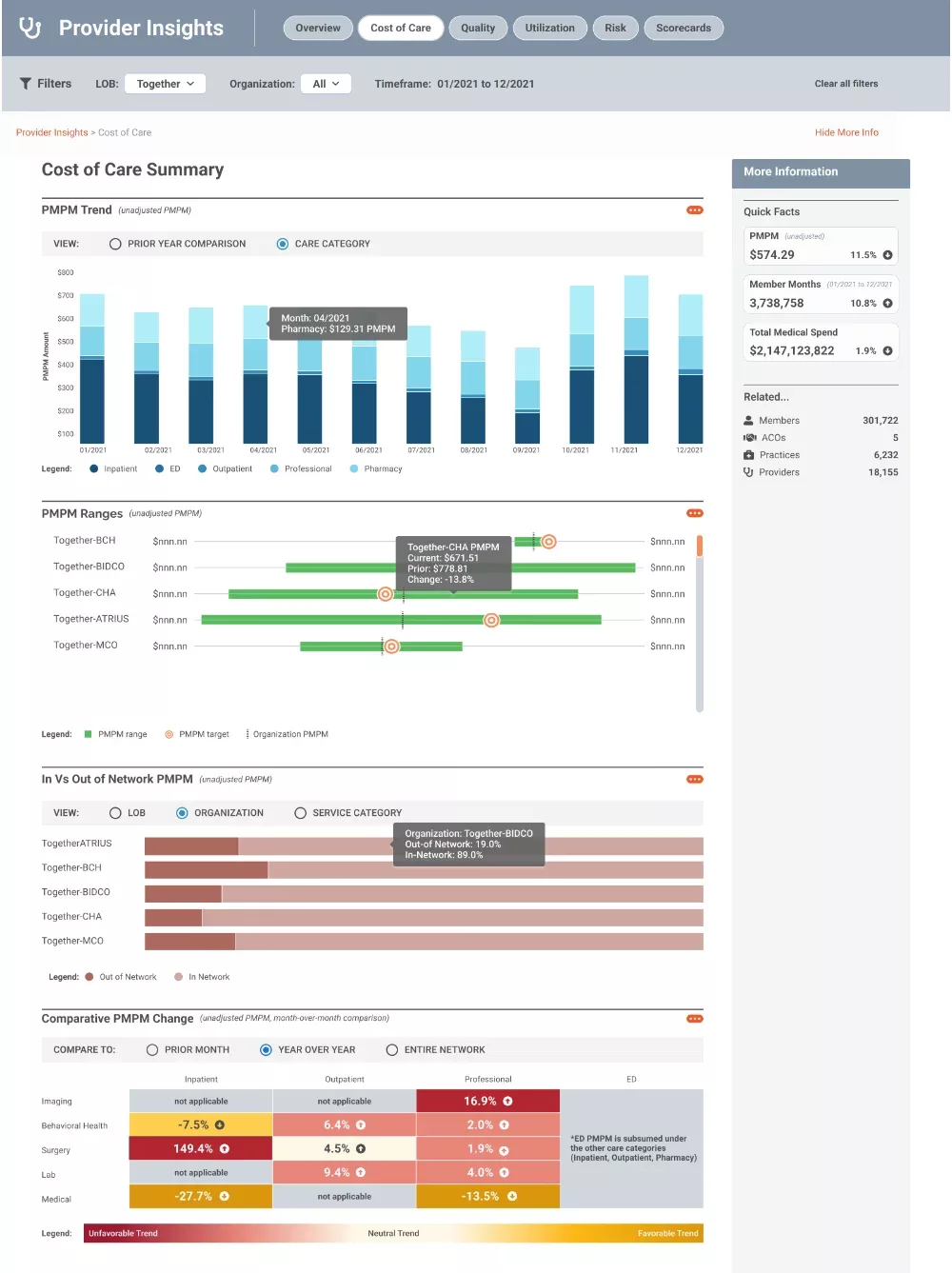
- Provider performance assessment: Access quality and utilization measures reports, compare performance across multiple practices and prioritize underperforming providers for targeted intervention.
- Provider performance monitoring: Identify drivers of adverse trends and outliers, provide ongoing updates and partner with providers to develop improvement programs.
- Patient care management: Review practice/provider performance against targets and engage providers in performance review to efficiently manage patient care.
Prevent and manage health risks with data-driven insights – target high-risk populations, understand contributing factors and prioritize interventions
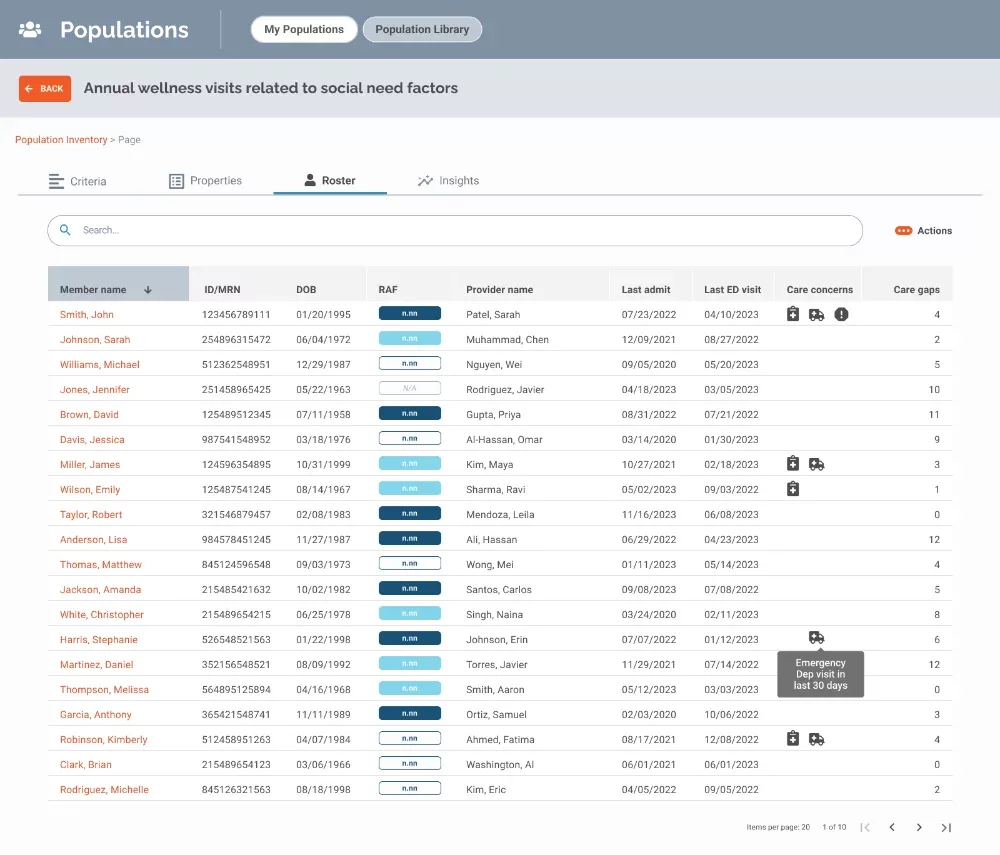
- Member screening and risk stratification: Identify patients for targeted interventions by efficiently screening and risk stratifying patient data based on various measures, demographics and practice/provider information.
- Patient assessment and education: Monitor interventions, identify performance gaps and root causes and prioritize high-value patient subgroups for outreach and management.
- Incentive program creation: Assess program and intervention effectiveness, track patient goals to gaps in care and identify high-value patient sub-groups for targeted management. Then create programs that will boost cost and quality performance.
Trusted by:


I’ve looked at several different tools, and CoreTechs® is the only one that brings in social determinants of health, contract management and population insights — everything we need to be able to manage contract and follow our patients to see where they are slipping through the cracks.
Gray Matter showed us how we could reduce manual referrals and accelerate care for patients with machine learning that identifies patients who require a referral based on clinical conditions and eligibility information.
Based on the reputation of the management team at Gray Matter Analytics and their ability to demonstrate their understanding of physician performance/value-based care, we decided to become their first CoreTechs® customer. The proof of concept is continuing, and we have very high expectations on the results.
CoreTechs® brought to the surface chronic conditions like diabetes that we had not coded. From that, we learned how to capture and document risk-adjusted factors for shared savings contracts and patient enrollment in disease management programs.
We were at a loss for why our members were seeing providers outside of our network. Gray Matter gave us the analytic tools to understand who would seek an external specialist, when and why. We learned the best points along the care continuum to intervene and even the dollars at risk for each member’s out-of-network choice.
Gray Matter Analytics developed models to help us predict members at risk of postpartum depression so we could proactively offer behavioral health services and take better care of our moms and their families while reducing costs.
Data-driven insights from CoreTechs® guided physician education, code capture, patient outreach and pre-visit planning to help us meet the quality, care and cost expectations of the Medicare Shared Savings Program.
Our team was stretched thin. Gray Matter became our advanced analytics partner and helped us with important work with analytical models and capabilities in CoreTechs® that would have taken years for us to develop on our own.
A lot of times there’s a disconnect between the provider and the payor. With Gray Matter Analytics, we’re looking at the same data.
