CoreTechs® Solutions
Assessment and onboarding
Take the first step toward success. We’ll conduct a rapid diagnostic of your value-based contracts, data and user groups while standardizing your data in an accelerated introduction to the CoreTechs® Solution. Working with you, we’ll bring conformity to diverse data from claims, EMRs, HIEs and other sources and allow you to see measures from your value-based contracts configured in our MeasuresLibrary®. Next, we’ll dig into your data to identify real, high-impact opportunities to increase revenue and improve quality. The onboarding process is designed to show you how the highly configurable CoreTechs® can elevate your performance and help you achieve better financial results and health outcomes.
[ MeasuresLibrary® ] consists of standard CMS and HEDIS measures preconfigured to quickly address your contract requirements.
Analytics solutions
Optimize performance through foundational, self-service advanced analytics. Upon completion of the CoreTechs® onboarding process, we’ll work with you to transition to a subscription. Our analytics as a service (AaaS) model ensures you have access to the latest user-friendly technology and insights, integrated into your existing workflows, without having to invest in expensive infrastructure. CoreTechs® uses AI to curate member outreach for optimal financial performance, risk mitigation and contract performance as well as to better inform care decisions. Because our solution is cloud-based, you can access it at any time, anywhere, without having to worry about interoperability or integration.
Analytics services
Health systems and plans have limited resources to meet value-based contract requirements. Let us be an extension of your team, providing additional support where you lack resources or expertise. To ensure that you get the greatest value from CoreTechs® and the insights you receive, our analytics services team works with you to optimize visibility of relevant data and prioritize action that will get results. Our subject matter experts help maximize the benefits of your subscription and guide the form, execution and evaluation of efforts to improve outcomes and address cost optimization in the delivery of care in a complex healthcare landscape.
See current and past contracts for analysis of best practices and performance comparisons to inform current care delivery, management and future contract negotiations.
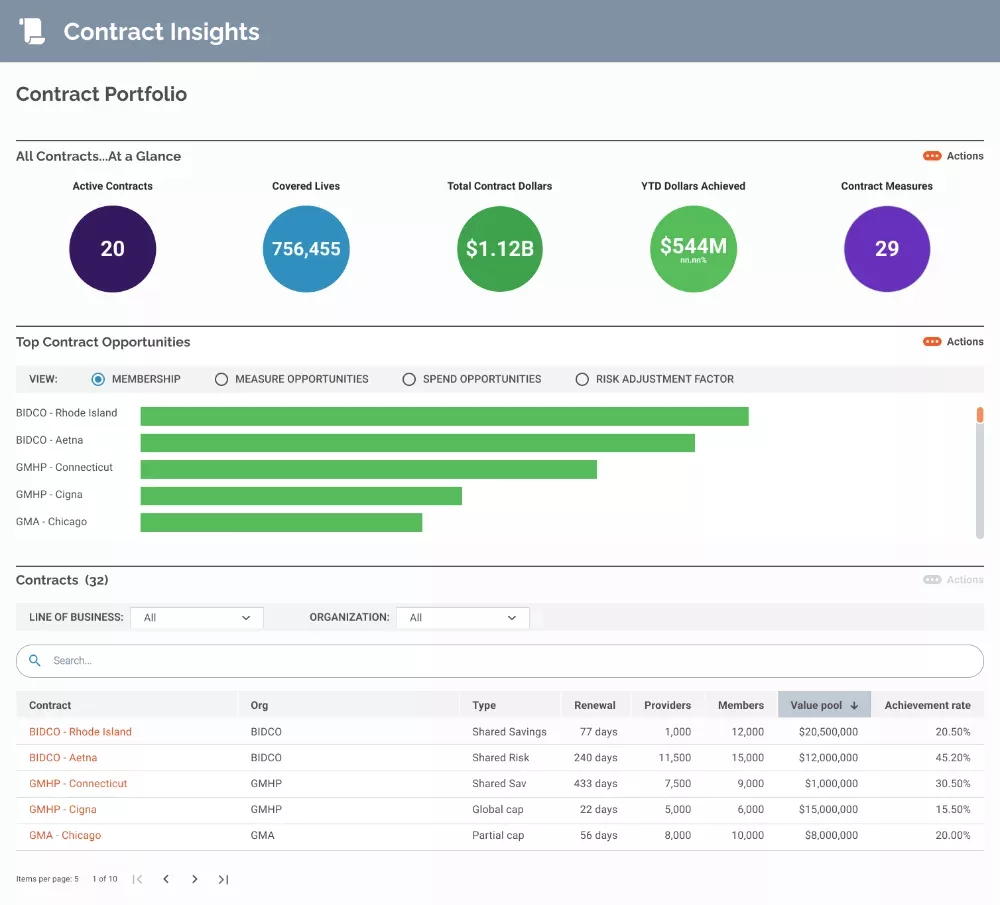
- Plan and optimize resource deployment for care gap closure across contracts or within a single value-based arrangement.
- Use predictions of the likelihood for success on value-based contract measures to forecast contract revenues at term end.
- Observe performance strengths and weaknesses to inform future contract negotiations.
Maximize the effect of value-based care with a holistic view of performance across different healthcare measurement areas, such as HEDIS, cost, utilization and health equity.
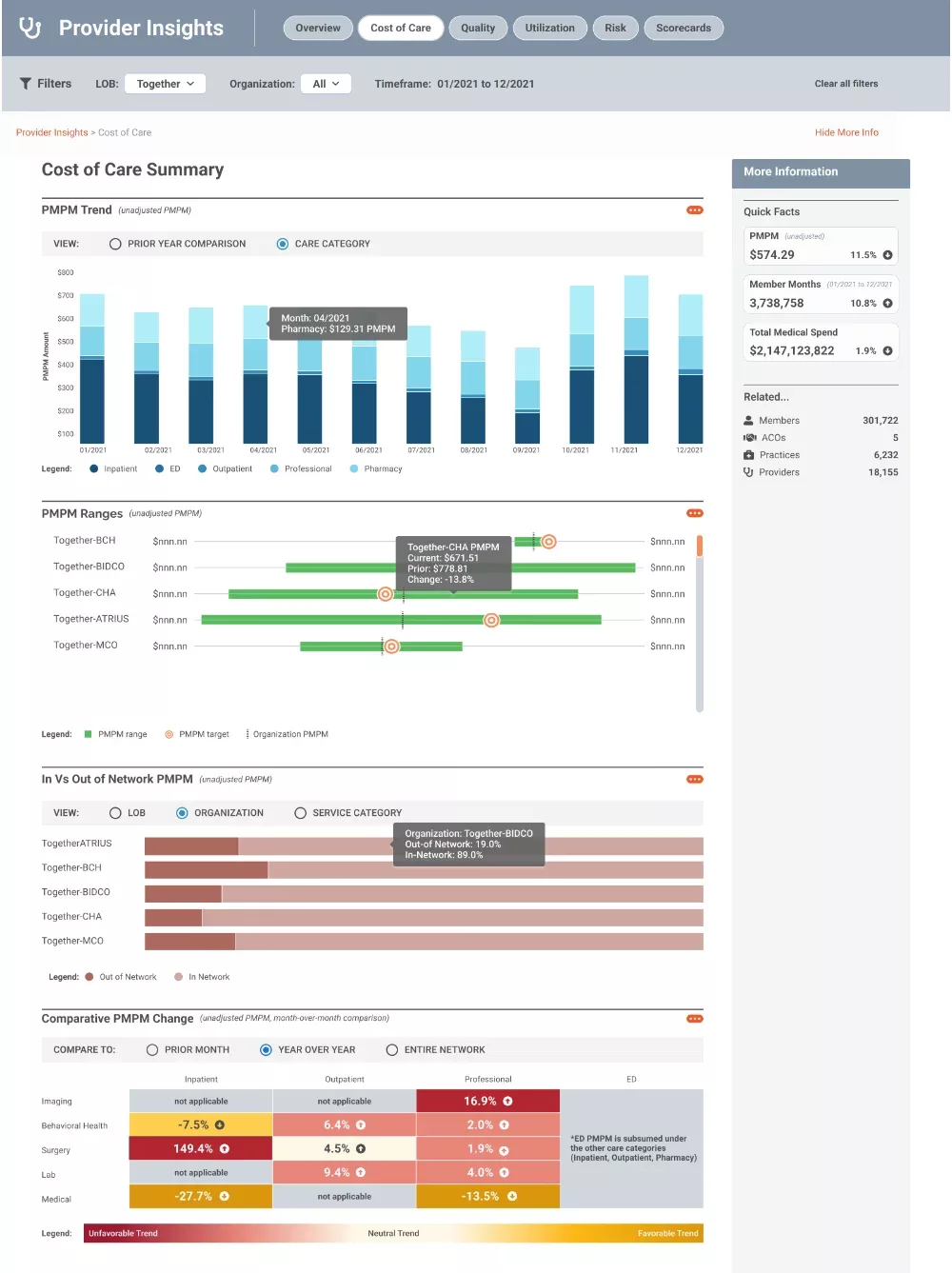
- Understand Cost of Care and other metrics in user-friendly visuals.
- Identify outliers and detect negative cost trends across categories, high-impact services, practices and providers.
- Monitor the factors influencing performance, such as inadequate management of chronic diseases, lack of follow-up care, dropped Hierarchical Condition Category (HCC) codes and social determinants of health.
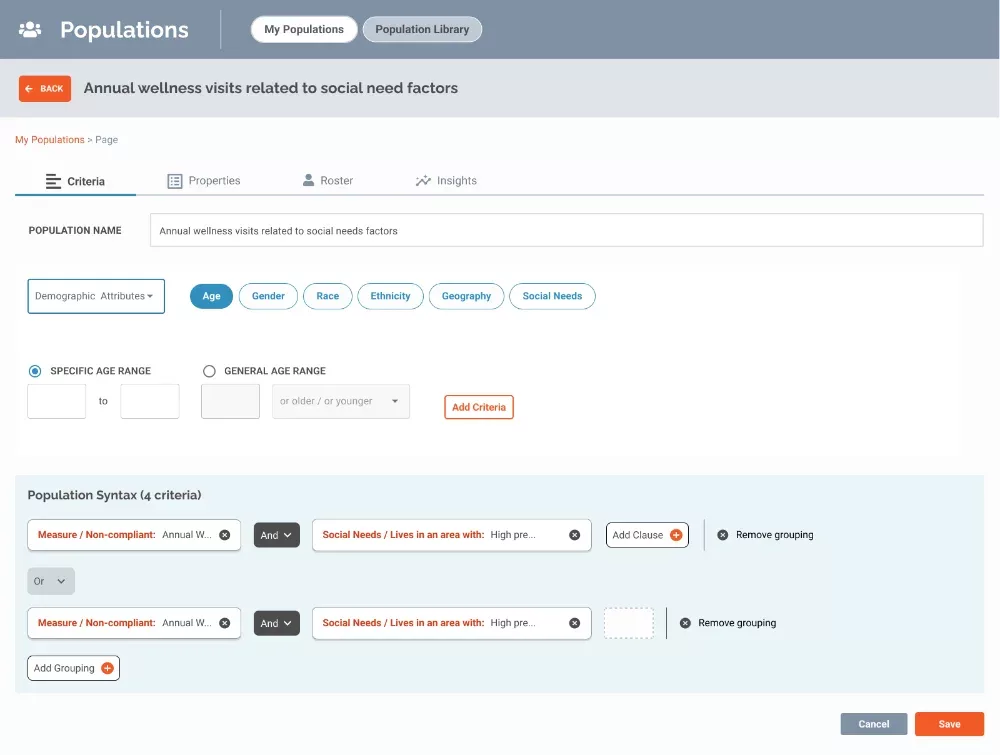
Generate strategies for individuals and populations at risk, aligning with expectations of commercial, Medicaid and Medicare value-based contracts.
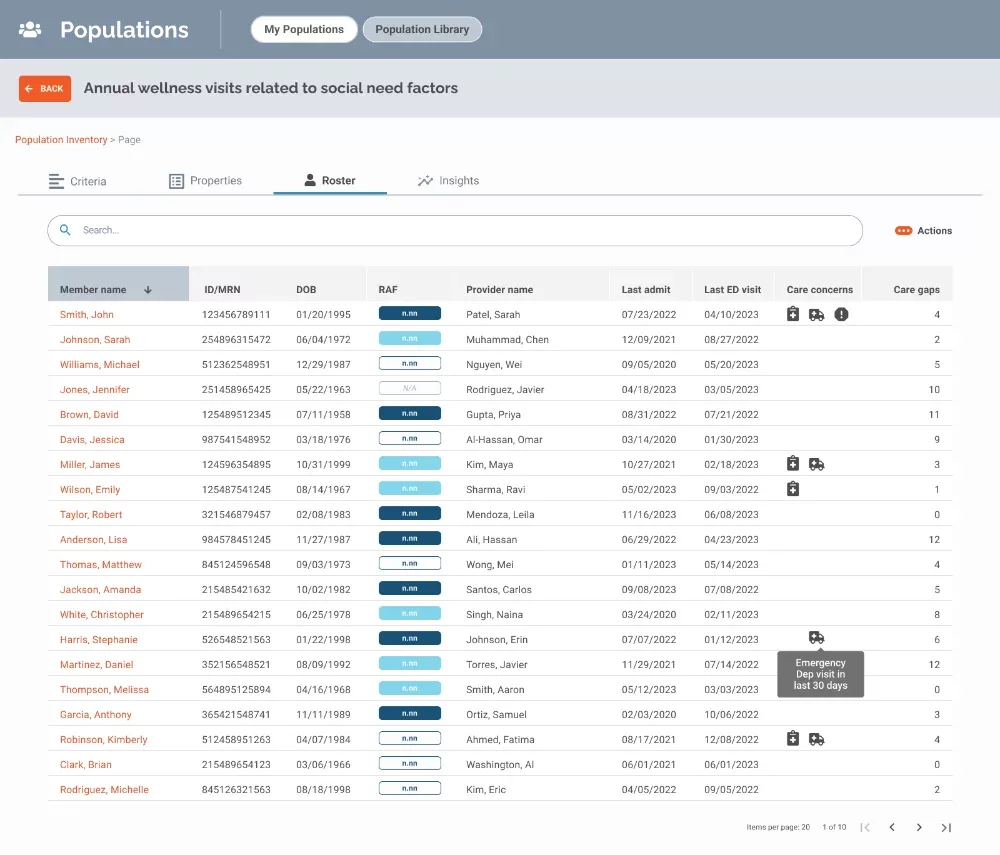
- Leverage self-reported health equity disparities and social determinants of health factors to improve outcomes.
- Create populations for intervention based on high-cost contributions resulting in poor performance such as avoidable emergency department visits and missed Hierarchical Condition Category (HCC) codes.
- Target communications to drive more specific diagnoses and guideline-adherent treatment as part of risk adjustment efforts.
To learn more about how SDoH impacts value-based care, check out Cracking the Code on Social Determinants of Health Data
Trusted by:




I’ve looked at several different tools, and CoreTechs® is the only one that brings in social determinants of health, contract management and population insights — everything we need to be able to manage contract and follow our patients to see where they are slipping through the cracks.
Gray Matter showed us how we could reduce manual referrals and accelerate care for patients with machine learning that identifies patients who require a referral based on clinical conditions and eligibility information.
Based on the reputation of the management team at Gray Matter Analytics and their ability to demonstrate their understanding of physician performance/value-based care, we decided to become their first CoreTechs® customer. The proof of concept is continuing, and we have very high expectations on the results.
CoreTechs® brought to the surface chronic conditions like diabetes that we had not coded. From that, we learned how to capture and document risk-adjusted factors for shared savings contracts and patient enrollment in disease management programs.
We were at a loss for why our members were seeing providers outside of our network. Gray Matter gave us the analytic tools to understand who would seek an external specialist, when and why. We learned the best points along the care continuum to intervene and even the dollars at risk for each member’s out-of-network choice.
Gray Matter Analytics developed models to help us predict members at risk of postpartum depression so we could proactively offer behavioral health services and take better care of our moms and their families while reducing costs.
Data-driven insights from CoreTechs® guided physician education, code capture, patient outreach and pre-visit planning to help us meet the quality, care and cost expectations of the Medicare Shared Savings Program.
Our team was stretched thin. Gray Matter became our advanced analytics partner and helped us with important work with analytical models and capabilities in CoreTechs® that would have taken years for us to develop on our own.
A lot of times there’s a disconnect between the provider and the payor. With Gray Matter Analytics, we’re looking at the same data.
