Medicare’s Readmission Penalties Just Hit New High, Now What?
A recent report from The Centers for Medicare & Medicaid Services, CMS, highlighted a sobering trend; for FY 2017, most of the nation’s hospitals are going to pay penalties under their readmission program. In layman’s terms, hospitals are discharging patients before their vital health conditions are stable, and therefore, the patient requires hospital readmission within 30 days of discharge. For such cases, the government imposes penalties on the hospital.
What do penalties mean to hospitals: Lost revenue and opportunity
From October 2014 through September 2015 (federal fiscal year), penalized hospitals will see CMS reducing payments for a patient stay. These penalties apply to patients admitted for any condition, not just the five conditions – heart failure, heart attack, pneumonia, chronic lung problems such as emphysema and bronchitis, and elective hip and knee replacements, used in determining whether a hospital has too many readmissions.
As an example, if Medicare normally pays a hospital $15,000 for a kidney failure patient, under a 1.5 percent penalty, Medicare would deduct $225 and pay $14,775. This penalty does not apply to Medicare payments that compensate hospitals for their general operating expenses, the training of medical residents or the treatment for low-income patients.
The growing complexity in reducing hospital readmission
Reduction in readmission rate depends on so many factors and many of them are out of hospital’s control.
A new study published in the Sept. 14 edition of JAMA Internal Medicine, found that hospitals with high readmission rates are being penalized “to a large extent based on the patients they serve,” not as a result of care deficiencies during a hospital stay. The study identifies patient sociodemographic factors, such as income, education, occupation, and primary language, as highly influential in determining whether a patient is readmitted to the hospital.
Under Medicaid Savings Programs, when low-income patients receive treatment and are discharged, it’s often difficult for doctors to monitor patients because they don’t follow post-discharge instructions. Unfortunately, post-discharge complications are compounded further when patients cannot afford prescribed medication.
We cannot deny there are internal factors affecting elevated readmission rates. Given workforce shortages, greater access to care, and growing administrative and technical demands on practitioners, there are times when patients get discharged with unstable conditions. As a result, often a patient doesn’t get proper follow-up instruction or more education surrounding early-alert signs and symptoms. According to the Journal of General Internal Medicine, 1 in 5 hospital patients are discharged with unstable vital signs — a likely cause of deaths and readmissions.
2017 Readmission Penalties: A growing problem
From the CMS report, several alarming figures jump out.
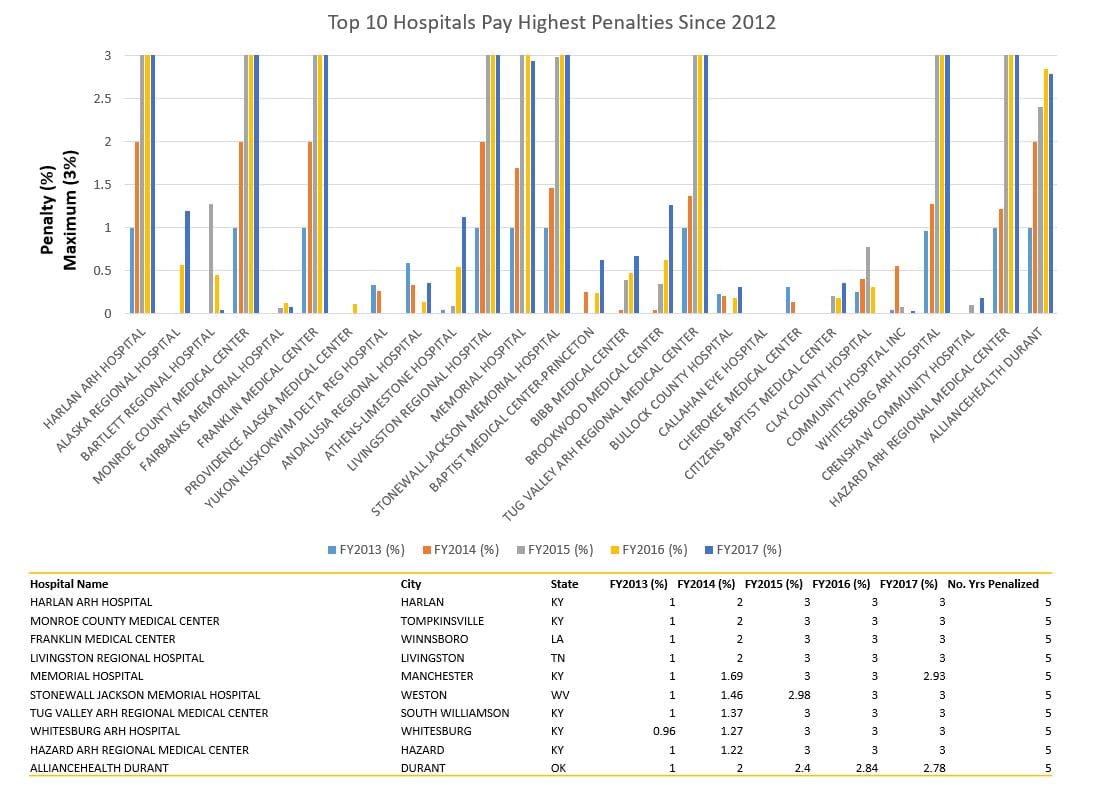
- 2,597 hospitals will be fined in FY 2017
- 1,621 hospitals have been fined 5 years in a row
- Penalties are expected to total $528 million, about $108 million more than last year
- 49 hospitals received the maximum fine (3%) – See below table
- The average reduction to hospitals was 0.73 percent for each Medicare payment, up from 0.61 percent last year
Clearly, the nation’s hospitals are struggling under Readmission programs. Innovative providers are turning to technology and analytics to improve their financial, operational, and care capabilities.
Stretched resources and growing big data demands requires hospitals to make the most of their investment in technology and analytics. To address readmission challenges. Best practices include;
- Identify patterns and conditions responsible for readmission using natural language processing – 80% of stored health information is unstructured, making it a challenge to sort and analyze the data. Utilizing natural language processing to extract key elements from unstructured history and physical, discharge summaries, echocardiogram reports, and consult notes can be useful to identify patterns which are responsible for readmission.
- Recommendation Engines Identify Chronic Disease Risk – Recommendation engines are common at eCommerce businesses like Amazon and Netflix. Similar engines in healthcare can provide personalized recommendations for health related treatments. Such recommendations engines could potentially reduce re-hospitalizations and increase healthy behavior engagement. Recommendation engine benefits include; a) personalized individual adherence regimens based on the nature hospitalization, demographic profile, self-reported behaviors, and other key variables. B) early detection and prevention of certain diseasesc) physicians can identify any signs during patient checkup and take preventive action to reduce risk of readmission.
- IOT and Telemedicine: Using Remote Monitoring to Reduce Hospital Readmissions – Physician can conveniently monitor a patient through a variety of applications and services using two-way video, email, smart phones, wireless tools and other forms of telecommunications technology. This allows physicians to monitor patients remotely. When a health condition arises, physicians will provide consultation through a phone or video conference, enabling early treatment before conditions worsen.
Use Cases
Using content analytics to identify preventative care opportunities, Seton Healthcare illustrates the value of NLP when used to extract key information from unstructured health data. As a result, they’ve been able to reduce readmission rates by identify high risk congestive heart failure patients.
The University of Virginia Medical Center in Charlottesville instituted a telehealth program that combines real-time data with remote monitoring for patients discharged with heart failure, pneumonia, COPD, a recent heart attack, or a hip or knee replacement. A technician sets up the equipment in the patient’s home within two days of discharge. The simple-to-use equipment consists of a small box that wirelessly transmits data from a blood pressure cuff and oximeter to a registered nurse. If the nurses notice any problems, they contact the patient by phone or, if needed, make an in-home visit. Just a year after implementing the program, the medical center saw its 30-day readmission rate drop to about 10 percent, compared to a national average of 17.5 percent (1).
Another telehealth benefit includes higher levels of patient satisfaction, seeing patients eliminate burdensome travel and the stress of waiting in the line. Increased patient satisfaction can also help hospitals to do better in value based payment programs (e.g. VBP, Hospital overall star ratings, etc.)
To solve the readmission problem, changes in policies and the introduction of new programs and initiatives include the following actions:
- Hospitals should reward physicians, nurses and other clinical staff for outperforming other departments for reducing readmission rates.
- Personalized Care and Attention – The responsibility of the hospital shouldn’t end with patient discharged. Assigned physicians and nurses should reach out to patients within a few days of discharge to see how they are doing.
- Design programs for low income and high need patients – Such patients are at highest risk of readmission. Hospitals can tailor plans for such patients by offering better discharge education, easier access to medication, and frequent monitoring and free examinations.
- Workforce Support – Hospitals must motivate physicians, nurses and other staff to submit their problems or concerns surrounding workforce shortages, workloads, time off, and stressful workplace environments. Such transparency and communication will increase workforce satisfaction and provide a better working environment.
Endnote
(1): http://altarum.org/health-policy-blog/telemedicine-using-remote-monitoring-to-reduce-hospital-readmissions